 |
| U of U Health patients now receive mammography results within 10 minutes of their scan. |
By Michael Mozdy
Not long ago, a woman getting routine breast screening at the University of Utah would wait an average of 6 days to learn her test results. Sometimes, she might be told to return for more imaging because there was additional information that the radiologist needed – further adding to the delay. A small percentage of women might have to come back yet a third time for a biopsy and wait for those results, too. This amounted to a significant amount of time and a heap of anxiety.
This scene is far from unique: nearly all breast imaging practices in the U.S. operate in this manner. Traditional mammography practices go through screening exams in batches because they believe this is the most efficient method. Sadly, it leaves patients wondering, worrying, and unhappy.
“Delay and anxiety are inherent harms in medicine,” claims Matthew Stein, MD, Chief Value Officer for Radiology and Imaging Sciences and Breast Imaging Section Chief. “Patients and physicians accept that there is a certain cost to be paid. What we might not realize is that some of these costs or harms can be avoided altogether if we can train ourselves to look at things in a different way.”
 |
| Matt Stein, MD, Breast Imaging Section Chief |
Only 5 -7 screens out of every 1,000 will detect cancer, so the vast majority of women will have normal test results. Much waiting and worrying is needless. Stein believes that reducing this anxiety is low-hanging fruit that radiologists can impact. “Less time waiting equals less time to experience anxiety, which equals less patient harm,” he declares.
One problem is that many think it can’t be done.
A Big Change for the Exam Room and the Reading Room
Stein trained in a program – the University of Washington in Seattle – where they gave a subset of patients their screening results the same day as their exam. He saw how much these women appreciated it, and he wanted to codify this process for the entire U of U breast imaging practice.
He gathered his team of radiologists, radiology technologists, medical assistants, and schedulers, and with the help of a U of U Health “value engineer,” they mapped out their entire process from the moment a woman calls for an appointment to when she is told the results of a biopsy if one was needed. They created an exhaustive process map, and identified the areas where time could be saved, and where the costs were located.
The team was not shy about their expectations. For the 94% of patients who have a normal exam result, the goal was just 10 minutes from exam to results (compared to 6 days). For those needing a biopsy of a suspicious area, the goal was 60 minutes from initial exam to biopsy.
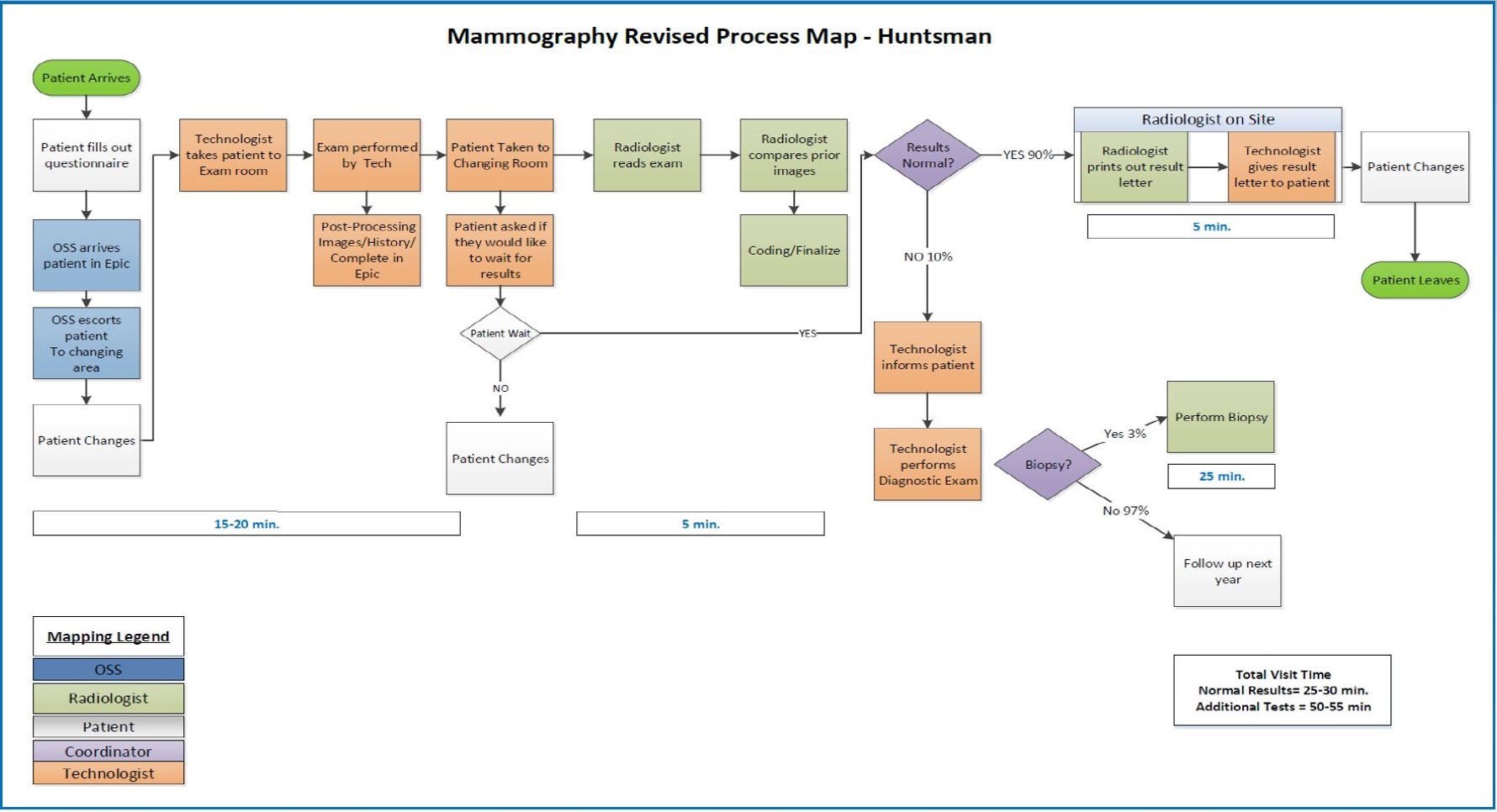 |
| The new process map for "screening with results." |
The process map they created is streamlined in terms of how exams are read and reported. In the updated process, the technologist calls into the breast radiology reading room with a single ring on the phone to alert the radiologist that a “screen with results” exam is ready. The radiologist pulls up the patient record, reads the images and then dictates and signs the finalized report. Signing the finalized report triggers a letter to be printed in the technologist work room. This letter clearly explains the results and any appropriate follow-up to the patient.
If the report is normal (as they are 94% of the time), the letter is then hand-delivered to the patient by the technologist. Therefore, the efficiency of the radiologist is not impacted the vast majority of the time, compared to traditional batch reading.
The remaining 6% of patients may have a suspicious area on the scan, may need more imaging, and may need a biopsy. The radiologist will speak personally with these patients, and additional tests and biopsies are done right then. The patient’s state of mind and anxiety level is always top of mind, and the radiologists carefully explain what they’ve seen on the scan and what the process will be like from this point forward.
This change means that the breast reading room must be staffed continuously from 7am-6pm (“It even makes you carefully plan your bathroom breaks,” Stein admits). Importantly, this attention to screening mammography represents a shift in how radiologists think of this type of test. “It’s a little change in dogma,” explains Stein, “because we elevate screening to the level of urgent or emergency care.” The whole team needed to commit to this new way of thinking.
Patients Speak Up
 |
| Stein discusses testing with a radiation technologist, Ashlee Roberts. |
The results of this new process are revealed in the data. First, the quality of scan interpretation has not declined, as some feared: the rate of cancer detection has remained the same with no increase in false positives, which may be thought of as “false alarm” testing. Stein feels that the breast imaging team is making more accurate determinations with the added knowledge that patients are waiting to hear their results. “The the stakes have been raised considerably,” he admits. If radiologists don’t have to immediately face the consequences of their interpretations, it may be tempting to simply order more tests. With the new process, however, the radiologist reading the scan must immediately follow through on any additional imaging or biopsies that he or she feels are necessary.
Second, radiologists have been able to manage the workload and new interrupted reading time without any added cost in terms of the length of their workday. They’re proud to report that they are hitting their goals: the vast majority of patients get their results in ten minutes or less.
Finally, patients are ecstatic. Here’s a sampling of actual patient comments from submitted surveys:
- “Thank you, thank you, thank you for having a radiologist read my x-rays immediately. It was such a joyous feeling walking out of my mammogram with the test results in my hand.”
- “LOVED, loved, loved the fact that the radiologist read the mammogram while I waited. This is a HUGE plus. No more anxiety waiting for the results! Kudos to whomever came up with the idea and implemented it. Thank you!”
- “I want to comment that having the radiologist read my scans immediately was super important. It was so much better to go home knowing my results right away, rather than having to wait a week. For cancer screening, I think this is critically important, since the wait can be agonizing.”
- “The most fabulous thing that happened during this experience was receiving my results within 5 minutes after the test. Further, my technician informed me that should I need something additional such as an ultrasound or biopsy, I would receive those immediately – no waiting. I can’t tell you how good this made me feel. A wonderful service.”
How Often to Screen?
Some have argued that routine screening should be delayed until age 50 and that less mammography should be performed (i.e., every other year, stopping at age 74, etc). A common harm cited is the false-positive exam, or a “false alarm” that results in patient anxiety, unnecessary testing, and increased costs. Another argument is that a woman might needlessly be treated for a cancer that won’t spread or otherwise affect her lifespan (called “over-diagnosis leading to over-treatment”).
Stein admits that the harms are significant and need to be carefully considered and diminished wherever possible. Yet amid disagreements, clinicians are all equally motivated by what they feel is best for patients. “That is the common ground in which we can work toward consensus: to maximize the proven mortality benefits of breast cancer screening, while working hard to minimize the harms,” says Stein. He strongly believes in yearly mammography screening beginning at age 40. “At the end of the day, my primary goal is preventing death from breast cancer.”
Treatments – chemotherapy, immunotherapy, radiation therapy and surgery – continue to evolve and improve. Over the past three decades, women have been presented with more options like breast-conserving therapies, which have the same outcomes and low recurrence rates as total mastectomy. Less invasive methods of treatment and diagnosis are constantly investigated. For example, another U of U Radiology and Imaging Science faculty member, Allison Payne, PhD, has created a new MUSE system that uses powerful ultrasound waves to burn (ablate) tumors completely non-invasively.
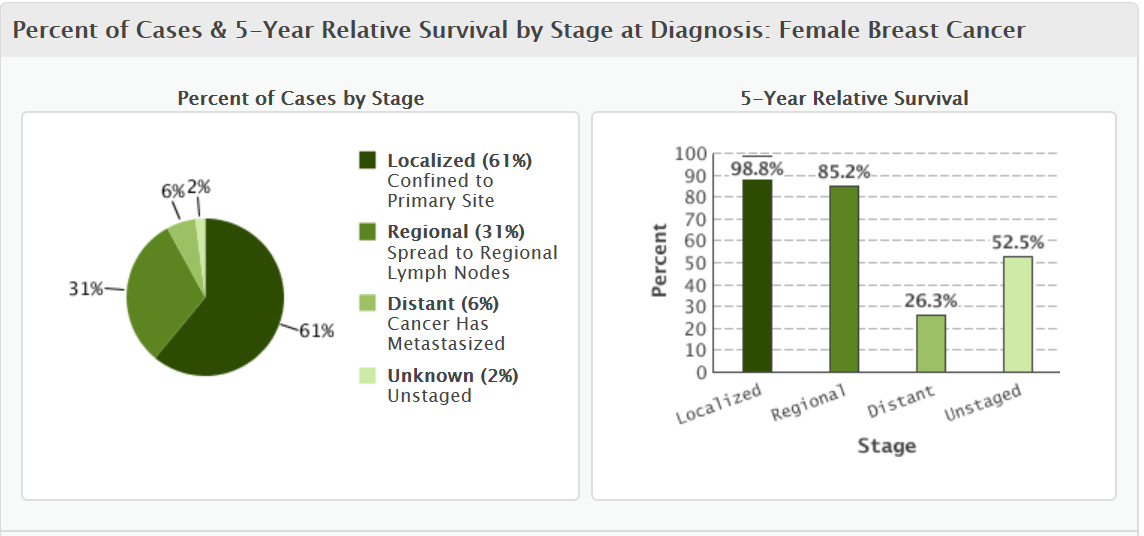
Fundamentally, radiologists like Stein firmly believe that mammography saves lives and is worth it. Simply put, when women are treated for early-stage cancer, their survival rate is great (98%), but if they don’t catch the cancer until later stages, such as when it’s obvious on a self-exam, survival rates plummet to just 26.3% for distant cancer that has metastasized (see graphs below, data from the American Cancer Society report "Cancer Facts and Figures 2016"). If screening can catch small, early-stage cancer, the result is that more women live longer.
One of the remaining criticisms of routine breast screening exams is that it increases patient anxiety. That’s precisely what Stein and the breast imaging division targeted with their new process.
The Future for Screening: Shared Decision Making
The truth is that women hear many conflicting pieces of advice on mammography screening. That’s why the breast imaging team is moving beyond the service of screening with immediate results to engage women in a personalized discussion of how often they should receive screening.
They’re focusing on a woman’s first mammography appointment because it’s the perfect opportunity to relieve some anxiety over what they’re facing in a new phase of life. The plan is to schedule a longer-than-normal appointment that includes a detailed family history, the possibility of genetic testing, the mammography screening itself, and then a personal meeting with a radiologist. The meeting with the radiologist is a valuable moment for a woman to discuss the particularities of her breast anatomy, scan results, family history, and genetics – all of which help the radiologist describe her specific category of risk. Hopefully, with this information, a woman will be able to make the most informed decision possible, and the radiologist can “step out of the shadows” and become a visible and valued member of the shared decision making team with the patient.
Stein is immensely proud of the way his team has come together and embraced the new “screening with results” process. The success of this first endeavor makes him very optimistic about the success of the “shared decision making” model: “It’s cliché but completely true,” he says with a smile, “it takes a village to do these things. I’m just extremely lucky to live in such wonderful village, surrounded by truly incomparable and caring colleagues and co-workers at UUHC and Huntsman Cancer Hospital”.
We look forward to seeing the shared decision making model in practice in the near future.