 |
| Members of the calf perfusion study: (standing in back) Vivian Lee, PhD, MD, MBA; Chris Conlin; Gwenael Layec; (seated on couch) Lorne Hofstetter; Christopher Hanrahan, PhD, MD; Jeff Zhang, PhD; Kristi Carlston; Kexin Hao. Missing from photo: Michelle Mueller, MD. |
By Michael Mozdy
Most of us are familiar with coronary artery disease, but arteries throughout our body – not just the heart – may build up plaque and narrow, reducing blood flow to the surrounding tissue. In the brain, it can lead to ischemic stroke, and in the legs, it leads to peripheral artery disease (PAD).
PAD is very common: 1 in 20 people over the age of 50 have it. It’s also a serious health condition – in addition to lowering quality of life, leg muscles can atrophy completely and patients risk gangrene and amputation. People with PAD are also at higher risk for stroke and heart disease; worse yet, in the more advanced stage of the disease, the risk of death is increased nearly 3-fold.
| Learn about PAD with this video from Open.Osmosis.org |
The treatment regimen is similar to coronary heart disease: medicines to lower cholesterol, prevent clots, and lower blood pressure; and in more severe cases, angioplasty and bypass surgery. But in some cases, even surgery hasn’t solved the problem. A more conservative approach has been to prescribe exercise, although it is difficult and seems counterintuitive to patients since exercise is precisely the thing that causes them pain.
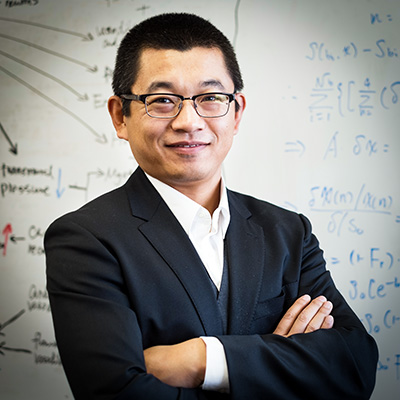 |
| UCAIR researcher and Radiology faculty member, Lei "Jeff" Zhang, Ph.D. |
One UCAIR researcher has set out to see if, in fact, exercise can be just as effective as medical treatments for PAD. If so, patients can be shown that it’s worth their effort to exercise through the pain. His name is Lei “Jeff” Zhang, and thanks to a great experimental design that pairs innovations from our College of Health faculty with magnetic resonance imaging techniques used in cancer care, he has received an NIH R01 grant to test this theory.
Testing over Time in Two Ways
Zhang’s approach is to examine the blood flow to muscle tissue in the legs, also called perfusion. In healthy adults, the heart pumps blood through the major arteries to the legs, and it is then carried to tissues like the calf muscles. But in people with PAD, we see a phenomenon similar to cardiac patients called “arterial steal” or “vascular steal,” where areas close to the larger arteries “steal” the blood flow that would normally go to peripheral areas because they’re trying to make up for blockages.
The result of arterial steal in PAD patients is that the superficial calf muscle, called the gastrocnemius, has poor perfusion because the blood pumped from the heart remains in the major leg arteries and therefore close to the major calf muscle, called the soleus. In patients with moderate PAD, their calf muscles can look normal although they experience pain when exercising because their muscles aren’t getting fed the oxygenated blood they need. In more advanced-stage PAD, calf muscles may be completely atrophied and replaced by necrotic tissue, and they often experience pain all the time, even when not exercising.
 |
| Gwenael Layec, Jeff Zhang, and Christopher C. Conlin (Ph.D. student). |
Zhang’s study will compare 40 PAD patients with 40 healthy, age-matched control subjects. His team will measure perfusion in the calf muscles at rest and at stress. They define rest as just a small wake-up call to the muscles as performed by some light exercise followed by a 4-min MRI scan while they remain still. Then, they spend about 10 min in progressively more strenuous calf exercise, until they feel exhausted, at which point, another 4-min MRI scan images their perfusion after stress.
This is the first way Zhang’s team is testing over time: how does perfusion change between resting muscle and stressed muscle? The second way is that they are bringing their subjects back after a 12-week exercise regimen to see if and how their perfusion changes. This data will tell them if exercise therapy has an impact on blood flow and perfusion in calf muscles of PAD patients, and therefore whether it is a viable treatment option for long-term health.
The Trick to Measuring Calf Muscle Perfusion
Zhang worked in Dr. Vivian Lee’s lab at NYU and came to the University of Utah with her. Lee is a world-class expert on using MR angiography to diagnose PAD. The techniques she developed allow clinicians to accurately know the location and degree of stenosis, or narrowing of an artery, so they can better perform surgery. While MR angiography provides a detailed structural picture of arteries, it does not reveal the amount of perfusion in the local muscle groups.
The challenge with visualizing perfusion is that the signal of blood as it moves into and through muscles becomes very small, and therefore difficult for an MRI machine to detect. Zhang knew that introducing a substance called a “contrast agent” to the patient’s bloodstream could boost the signal, so his proposal focused on this technique of dynamic contrast enhanced MRI (DCE-MRI). This contrast agent, gadolinium, is a non-radioactive, FDA-approved substance that the body processes and excretes within 24 hours. And once introduced, the DCE-MRI studies allow Zhang’s team to watch perfusion happen over a 4-minute window, and observe exactly how blood enters, spreads, and even diffuses out of muscles. Zhang concentrates on a 40-second piece of the study to create his perfusion maps.
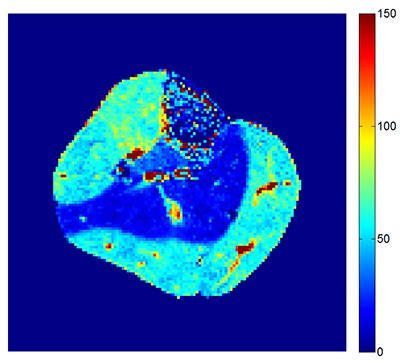 |
| "Heat map" showing perfusion in a cross-section view of a calf muscle - the red areas indicate more blood flow. |
In his preliminary work, the visualizations look great. The DCE-MRI technique does, indeed, help to capture perfusion in calf muscles in the 4 patients they studied. His work builds upon the structural MRI work pioneered by Lee and moves into functional MRI.
An Exercise Device from the Exercise Experts
The extra push calf perfusion needed to be detected by MRI comes in the form of exercise. As you might expect, when a patient walks, climbs stairs, or runs, the heart pumps blood to the leg muscles. This elevates the amount of perfusion that would be picked up in an MRI scan.
When deciding how exactly he could have patients exercise their calf muscles in close proximity to the MRI machine, Zhang’s group considered the broad range of talent and research going on within the University of Utah health system, and found that someone had already developed just the tool they needed.
 |
| Gwenael Layec's device used to exercise a patient's calf while in an MRI scanner. |
Gwenael Layec, Ph.D., is a faculty member in the Department of Internal Medicine (Geriatrics) and is a part of the Utah Vascular Research Lab, led by muscle expert Russell Richardson, who also has a faculty appointment in the College of Health’s Department of Exercise and Sport Science. Their team studies how oxygen is delivered and how mitochondria function in skeletal muscle. They developed a number of innovative contraptions to help isolate specific muscle groups and exercise them. The good news for Zhang was that they had already made a tool for the calf to perform plantar flexion (the natural movement of walking), which exercises the superficial gastrocnemius muscle – the one most impacted by PAD.
In another example of how the University of Utah’s innovative and collaborative spirit leads to better research, Layec and Richardson agreed to lend their device to Zhang’s team for their study. The best part of their tool is that it can be used while the patient is lying down with their leg inside the MRI machine, streamlining Zhang’s experimental design.
Time Will Tell
Zhang feels good about his experimental design and the promise of the techniques he’s using, but he’s quick to praise his team, especially Dr. Lee. “She has helped to revise my papers many times and went through every sentence of my grant proposals,” he says. “This is an amazing amount of work and attention from a mentor.”
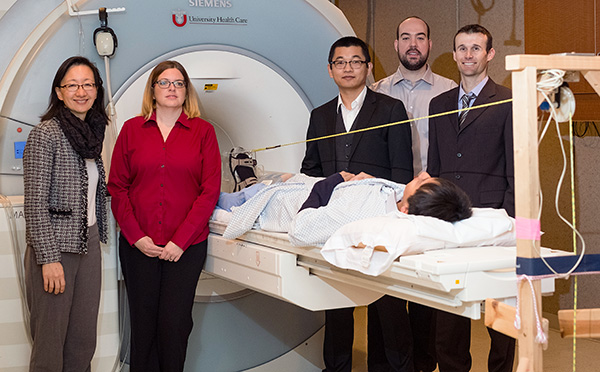 |
| Members of the team by the patient in the MRI machine (left-to-right): Vivian Lee, PhD, MD, MBA, Kristi Carlston, Jeff Zhang, PhD, Christopher Conlin, Gwenael Layec, PhD. |
As of January, 2017, Zhang is in the process of recruiting for his study. They expect that finding the 40 PAD patients to participate will not be difficult since we can refer these patients from our clinical system, but finding 40 age-matched healthy control subjects can be a bit harder. Kristi Carlson is the clinical research coordinator for the study, and anyone over the age of 45 who wishes to help advance the science behind PAD treatment can reach her at Kristi.carlson@hsc.utah.edu.