
University of Utah Health is First System in the Nation to Use 3D Augmented X-Ray Scans with Patients

By Michael Mozdy
Tiny, “hairline” fractures in hands and feet – more common than you might think – are very hard to see on medical scans. Often, patients must simply treat their injury tenderly and come back in a few weeks for another round of imaging if the pain persists. The difficulty in making a diagnosis is starting to change thanks to a much more comprehensive x-ray scan. University of Utah Health is the first and only health care site in the nation to be using Siemens Healthineers new 3D scan software with a motorized, telescopic x-ray machine.
The U of Utah Hospital was the first US system to install the Siemens Multitom Rax Twin Robotic X-Ray system in 2016 and it has allowed thousands of patients who are in pain or have mobility issues to be more easily scanned. This is because they can remain in a comfortable position while the machine is positioned around them. But the motors and software can do more than a traditional x-ray. Siemens Healthineers has received FDA approval to perform 3-dimensional, completely robotic scans of upper and lower extremities.
The 3D augmented x-ray scan is a completely different type of imaging study.
A traditional x-ray is a single shot that produces a flat image. X-ray technologists position patients to capture 6-8 different angles to try to best image a part of the body. The new robotic 3D scans use a movable x-ray source and independent, movable detector to quickly rotate around a body part and capture a near-continuous scan with about 30 images per second.
“We call this a ‘pulsed x-ray beam with continuous motion’,” explains Frederic Noo, PhD, a researcher at the Utah Center for Advanced Imaging Research who has spearheaded the use of this new technology at University Hospital. “It delivers much less of a radiation dose than a CT scan, which is a continuous beam with continuous motion, and it actually has much higher resolution.” Noo credits the smaller pixels in the x-ray detector, 150 microns in size versus 1500 microns in a CT scanner.
This new technology creates a composite image that is not just a set of flat scans: it is a true 3D image of the bones, appearing to the radiologists who interpret the scans much in the same way that a CT study would.

Maryam Soltanolkotabi, MD is a member of our musculoskeletal radiology section; her section chief, Dr. Megan Mills, and two of her colleagues, Drs. Hailey Allen and Amanda Crawford, have been deeply involved in the development and interpretation of these scans alongside Dr. Noo. They are very enthusiastic about their impact for patient care. “This new technology has been a great addition; it increases radiologist confidence in interpreting images and promises to help streamline patient care,” says Dr. Soltanolkotabi.
She explains that suspected fractures, difficult to see using traditional imaging, can negatively affect patient care. “Radiologists often communicate this degree of uncertainty with ED providers and request that patients come back in 10-14 days for a second set of radiographs to re-evaluate,” she elaborates. This represents a potentially unnecessary use of resources, time, and patient worry. “But augmented 3D technology lets us see those non-displaced hairline fractures. Patients don’t need to come back for a second set of imaging and both they and the ED providers get a diagnosis faster,” she says.

An augmented 3D x-ray scan provides a cluster of benefits: it is the first type of scan to truly detect hairline, subtle fractures (what radiologists call “occult” fractures), which results in a greater level of confidence for the radiologist interpreting the scan and thus a definitive diagnosis that allows ED providers to more quickly treat patients appropriately.
Emergency physician, Gerry Doyle, MD, has been impressed by the image quality of the scans, which he notes look like CT scans more than traditional x-rays. “We are really hoping that we can expand the use of this modality for patients who are at risk for fractures that may be missed on traditional x-rays due to anatomic issues, loss of bone mineralization or other factors,” he states.
Dr. Doyle brings up another benefit of the technology: while CT and MRI scanners are often busy and “relatively oversubscribed,” he says that being able to use the 3D augmented x-rays “might be faster and more readily available, and will help us avoid ‘missed fractures’ while maintaining ED patient throughput.”
Dr. Noo and other researchers at UCAIR have worked closely with Siemens Healthineers for decades. We are the first site in the United States to be using Siemens’s updated technology with patients (what they call “Real3D”) thanks to our strong collaboration with the company. We are using it for patient care and providing feedback to them about how it is working. The long-term plan, of course, is to use these improved scans regularly in the future, especially for emergency and urgent care situations.
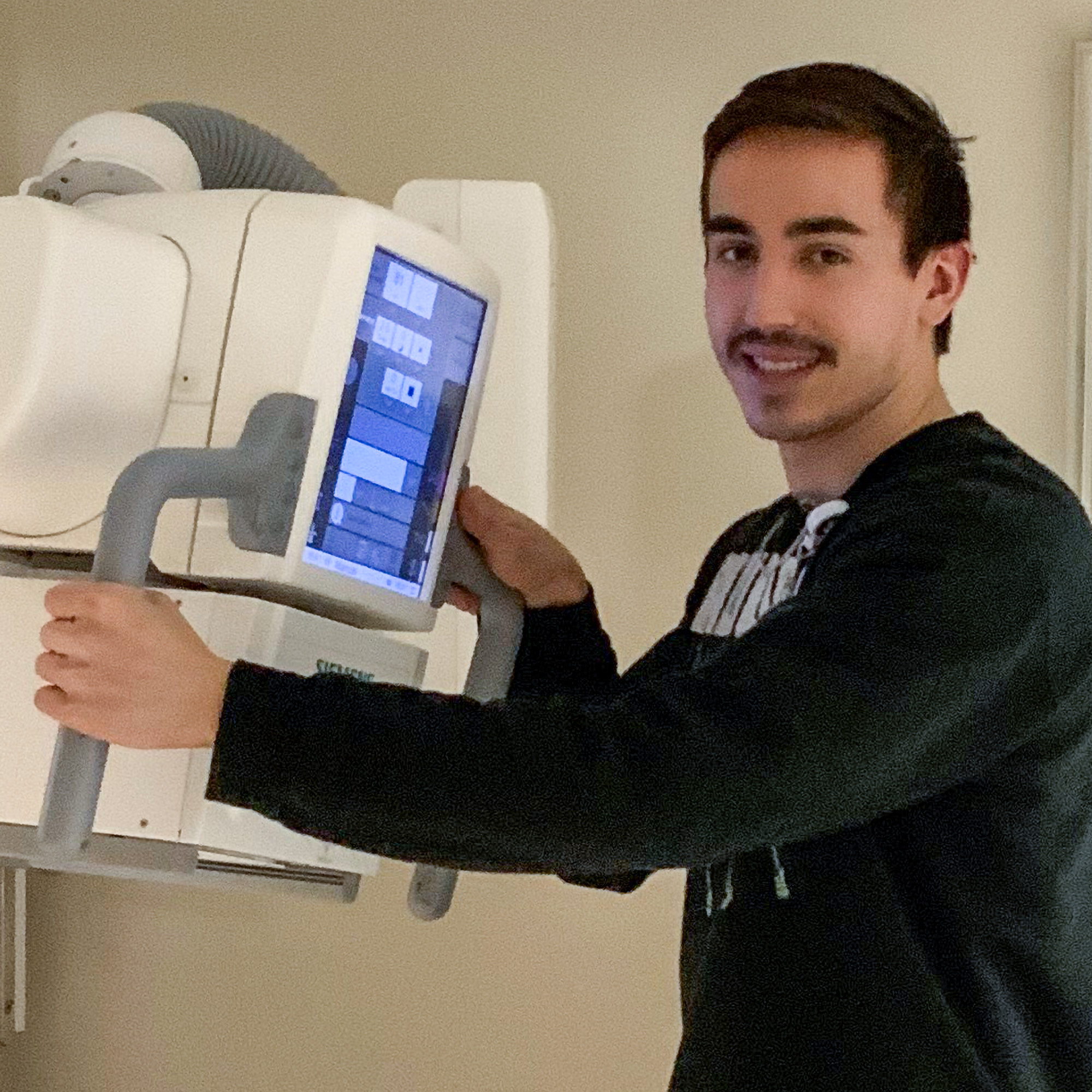
Dr. Noo and Dr. Allen worked with the X-ray team leadership on translating 28 commonly ordered scans of the extremities (hands, wrists, elbows, knees, ankles, and feet). He is very appreciative of the support and enthusiasm from the x-ray technologists at University Hospital, particularly Matthew Houser, who volunteered to perform our first scan on a patient. These scans can actually take less time in the x-ray suite than taking traditional radiographs because the x-ray technologists don’t have to re-position patients multiple times in order to achieve the correct angles.
To increase the uptake in ordering these new scans, the x-ray technologists called ordering physicians to explain how the new scans could provide even better information than the traditional x-ray scans they ordered. Slowly but surely, the ordering providers, radiologic technologists, and radiologists all grew accustomed to and appreciative of the new scans.
“Five years from now, I could see this type of scan replacing traditional x-ray and CT for imaging the extremities,” claims Noo.
Dr. Soltanolkotabi agrees and sees the utility in other areas as well: “In rheumatology, we will be able to see bony erosions around the joints much more easily and hopefully guide patient management by being able to assess disease progression or response to treatment more accurately.”
Improvements like this scan technology illustrate how radiology is an important intersection for research and clinical care. “Radiology truly is the engine that drives modern medicine,” states Satoshi Minoshima, MD, PhD, the Anne G. Osborne Chair of Radiology and Imaging Sciences. “I am very proud of Dr. Noo for pursuing this important new technology within our system, of the radiologic technologists who have worked to make it a reality, and of Dr. Soltanolkotabi and the musculoskeletal radiology section for demonstrating how clearly it can impact patient care.”